With four children and six grandchildren over for the holidays, Christmas was a busy time for Charleston resident Joanne Gilmore – one she normally looks forward to. The past few years, however, the 80-year-old hasn't been feeling herself.
“I kept thinking my legs didn't feel good because I was standing on them so much when I was decorating a tree and taking kids shopping,” she recalled about the holiday season in 2024.
By January 2025, she underwent an anterior cervical discectomy and fusion (ACDF), a neck surgery that could relieve pressure on her spinal cord and nerves – a step she hoped would ease her symptoms.
But instead, following her surgery, the left side of Gilmore’s body was immediately paralyzed. After nine weeks of inpatient rehabilitation following her initial ACDF performed at an outside institution, she was sent home from that hospital, despite her condition worsening and affecting her dominant side. She required a wheelchair and help with daily activities, and she could no longer take care of her two special-needs grandchildren, whom she watched while their mom was at work.
“I couldn't feed myself. I couldn’t do anything,” she explained. “I had no purpose in my heart to live that way.”
Fast forward a year, and Gilmore is now walking with a cane. Over the most recent Christmas holiday, she baked 10 varieties of cookies – all thanks to a second surgery – this one performed by MUSC Health spine neurosurgeon and physician-scientist Jamie Wilson, M.D., in June 2025.
“If you talk to people who are close to me, when they walk with me and see me now, they just sit back and are amazed,” said Gilmore. “They cannot believe the progress that I've made.”
Regaining function
Although Gilmore’s experience with her first surgery was dismaying, she decided to press on.
“I said I have nothing to lose at this point,” she said. “I have only things to gain.”
That led to her consultation with Wilson, who routinely treats patients in Gilmore’s situation.
“She was disappointed at the outcome of her first surgery,” said Wilson, “and in her desperation sought advice from MUSC as a last resort.”
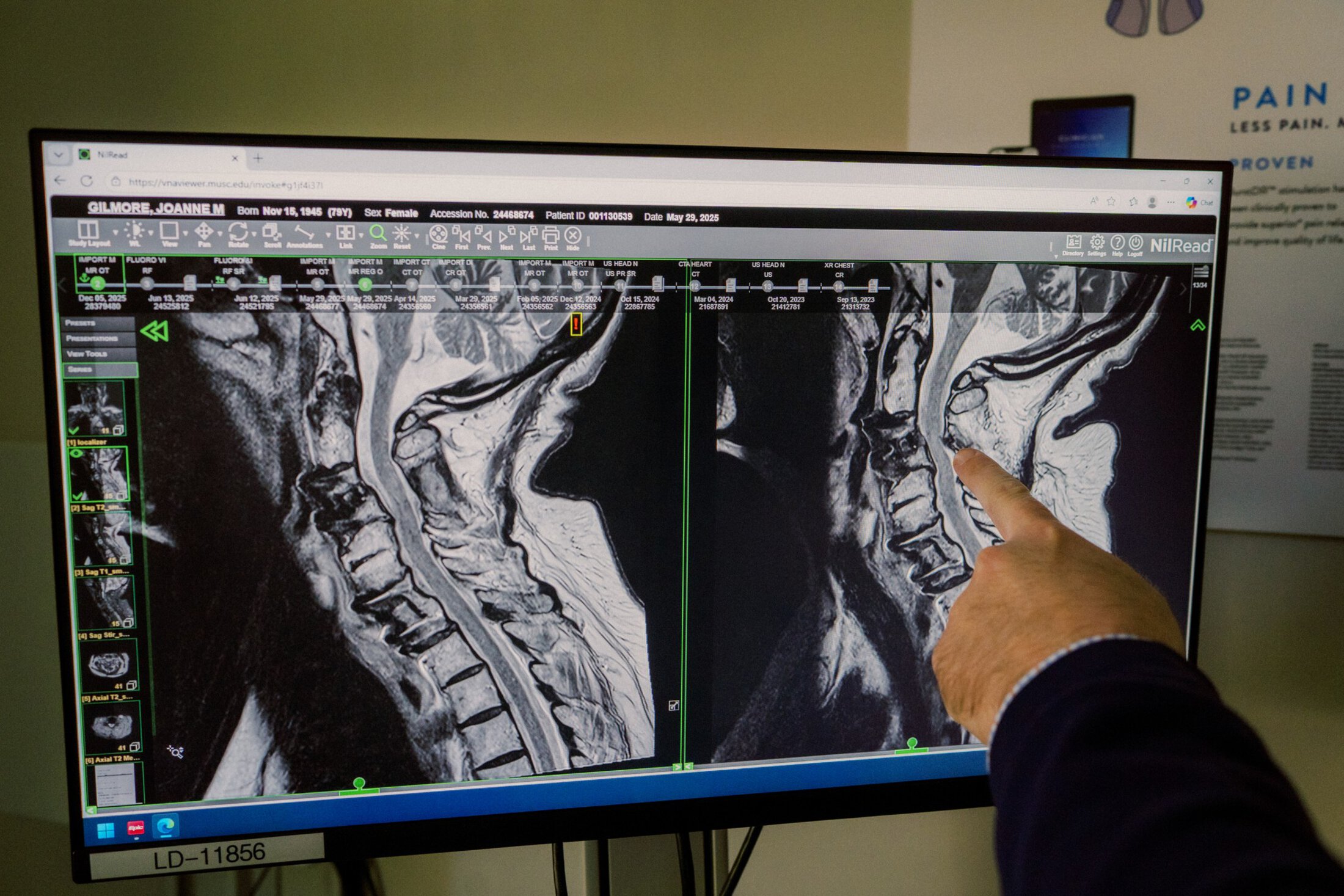
Wilson performed a laminectomy, in which he removed the bony arch at the back of the vertebra to enlarge the spinal canal and reduce pressure on the spinal cord and nerve roots. He approached the spine from the back of the neck to avoid the site of her previous surgery.
“Under the right circumstances, it can be a straightforward surgery. It takes about an hour,” said Wilson. “I do this a lot in my elderly patients with poor bone quality. It was a very, very good surgery for her, and she just recently had a post-operative MRI scan that shows she's had a remarkable improvement.”
Rehabilitation to further her gains
On the first day post-surgery, Gilmore could move the left side of her body for the first time in months.
With such promising initial signs, Gilmore committed herself to rehabilitation.
“I do rehab every single day,” she said.
And, thanks to the dedication of her occupational and physical therapists, Gilmore said she has regained the ability to feed herself and shower on her own. Most recently, she started driving again. Her progress comes as no surprise to Wilson, who noted that rehabilitation helps to promote brain plasticity – the rewiring of the brain to regain function.
“Her mobility is going to define the length of her life,” he said. “And, I explained to her how her mobility is so crucial to her staying well and staying active.”
Gilmore estimates that she has regained 75% to 80% of her original functioning. Looking forward, she hopes to regain sensation in her hands and feet. Wilson said the full extent of Gilmore’s recovery may take up to two years, due to how the nervous system typically recovers from injury.
“It's not the nerves themselves repairing and regenerating because they can't,” Wilson explained. “It's your brain rewiring, which is going to take a long time.”
Wilson is pleased with Gilmore’s clinical improvement but is careful to temper expectations when counseling her.
“There's a possibility that a patient in this situation might not get a full recovery,” he cautioned. “But your chances of making a better recovery improve if you seek help as soon as possible.”

‘Maximize the outcome, minimize the impact’
In the final analysis, Wilson thinks that Gilmore was both a good and a poor candidate for surgery.
On the one hand, he explained, she was very healthy and athletic before the ACDF. A self-proclaimed “gym rat,” she had strong social support and good cognitive functioning – both of which were in her favor.
On the other hand, he said, Gilmore was in a wheelchair and not able to move her arms and legs very well because of the spinal cord injury. But despite Gilmore’s condition, Wilson was still able to make a positive difference in her mobility and life. Wilson often helps patients with chronic nontraumatic spinal cord injury who are more difficult surgical candidates than Gilmore.
“Part of my research is in elderly spine surgery and maximizing outcomes in elderly spine surgery,” said Wilson. “So, my experience is being able to maximize the outcome and minimize the impact and being able to tailor the approach so that people can not only get the most out of the surgery but get back on their feet as quickly as they can.”
Wilson has spent his career researching biomarkers for frailty and advising patients to consider spinal surgery even if they’re frail. He encourages patients beyond South Carolina to reach out to MUSC for help and also hopes to establish a fellowship program in elderly spine care at MUSC. This program would train the next generation of neurosurgeons to treat chronic nontraumatic spinal cord injury, an underrecognized and underfunded condition that affects between 1% and 3% of the U.S. population older than 70.
“My long-term goal in five to 10 years is to try to make MUSC a center of excellence for elderly spine care,” said Wilson. “If you identify it early and get in there and do the surgery early, people really can regain their function and improve their quality of life.”
Looking forward
With her regained strength and mobility, Gilmore hopes to help others who may be wary of having spinal surgery. For instance, she advised her friend’s sister, who has neck and back problems, to see Wilson.
“He looks at you with concern,” said Gilmore of Wilson.“His rapport brings you comfort.”
With a newfound lease on life, Gilmore has many plans for the upcoming months. She was thrilled to be back to baking over the holiday season and hosting guests. She also hopes to travel again and return to her volunteer work as a chaplain. She credits her surgeon for giving her back the life she loves.
“Dr. Wilson saved my life.”